This product is available to purchase
Magnesium – Leptin ** Obesity and Diabetes
In my view, unless you nourish your body correctly and “not go for quick wacky ways of losing weight”, your battle will continue. Your body is your temple, and the most important vehicle you will EVER have to move around and LIVE IN during this life on earth. Regardless of what you have done with your body over the years, it is very forgiving and WILL become better with your better management of it.
******
The composition of basic foods or nutrients that most people eat today is vastly different from what early humans consumed a century ago.
One would think that eating too much would result in an abundance of nutritional support for cells. But being overweight and undernourished at the same time is a reality that is just beginning to be understood. It is quite strange to say to people that the more they eat, the more malnourished they are destined to be.
Overweight people more often than not suffer from gross malnutrition because the nutritional values of the basic foods available to us have been steadily dropping for the last 50 years even as toxic exposures increase. Obese people tend to eat too many processed white foods with a lack of essential vitamins and minerals.
 Excessive calorie intake is the fast track to lepton resistance. Since it’s hard to eat excess of the so-called “clean” foods, excess calories usually come from junk foods as do magnesium deficiencies.
Excessive calorie intake is the fast track to lepton resistance. Since it’s hard to eat excess of the so-called “clean” foods, excess calories usually come from junk foods as do magnesium deficiencies.
When dieters starve themselves of calories, they starve their brain cells as well.
New research finds that these hungry brain cells then release “feed me” signals, which drive up hunger, slow down metabolism and thus cause diets to fail.
Neurons sense nutrients in the body and tell the body when it’s time to eat and time to stop eating. The point is …… dieters are not just starving themselves of calories, they are starving themselves of vital minerals and this comes on top of already existing mineral deficiencies that are characteristic of overweight and obese populations.
Obesity is Starvation
Obese people generally have hyper-insulinemia (high levels of insulin in the blood) and insulin causes fat to be stored in fat cells.
Obese people in general cannot satisfy their body’s demands for energy or nutrients by eating.
In this scenario, lethargy, hunger and stress are not a cause of obesity; they are the effects or results of it (due to the internal starvation).
Syndrome X, also known as metabolic syndrome is a combination of insulin resistance, leptin resistance and glucose intolerance. All of these conditions are precursors to diabetes, heart disease, obesity and cancer.
Leptin and Magnesium
The new fashion in obesity is to look at the role of leptin, but what we are going to do in this essay is look not just at leptin but also at the leptin-magnesium axis that speaks volumes more than looking at either of these substances alone.
High levels of leptin seem to be related to increased urinary magnesium loss in patients with type-1 diabetes.
Hypomagnesaemia and hyperleptinemia are common in patients with diabetes. Moreover, it has been demonstrated that leptin stimulates diuresis and natriuresis causing the urinary magnesium loss in type-1 diabetes. Human leptin is a protein of 167 amino acids. It is manufactured primarily in the adipocytes of white adipose tissue, and the level of circulating leptin is directly proportional to the total amount of fat in the body.
Magnesium makes dieting easier by supporting the brain’s sensitivity to leptin.
Magnesium’s benefits go on forever it seems. Now we have to get serious and introduce it to the world of diet, weight loss and the medical science of obesity and diabetes.
Studies have shown that leptin and magnesium both play significant if not primary roles in
- heart disease,
- obesity,
- diabetes,
- osteoporosis,
- autoimmune diseases,
- reproductive disorders,
- and perhaps the rate of aging itself.
Many chronic diseases are now linked to excess inflammation such as heart disease and diabetes. High leptin levels and low magnesium levels are extremely pro-inflammatory.
Leptin
Leptin is a hormone that triggers your sense of feeling full. A leptin deficiency can cause overeating, leading to obesity and obesity-related disease.
Most people don’t have a leptin deficiency – they have lost their sensitivity to leptin, which is called leptin resistance. Much like insulin resistance, it’s possible to have enough leptin, but because your body doesn’t use it effectively, you still feel hungry. Leptin resistance is a serious health issue. Essentially you are overfeeding your body but the perception from your brain is that you are starving because you actually are missing vital nutrients such as magnesium.
Obesity and type-2 diabetes epidemics have joined forces ravaging the health of hundreds of millions of people around the world who have been significantly affected by this deadly pair. It is extremely important to understand how these two epidemics are intertwined.
The popular belief is that if one eats too much sugar, they’ll get fat and develop diabetes, but this is only half the truth. There’s more to the obesity-diabetes connection than what most doctors and just about everyone else typically believe.
When leptin is working properly it prevents nutrient spillover by telling insulin to shut off after your tank is full.
Every time you eat excess food (more than what your body needs for energy), leptin and insulin levels surge.
Leptin resistance leads to insulin resistance which further establishes leptin resistance.
Leptin levels correlate with insulin levels (both are high in hyperinsulinemia). The journal Circulation showed that men with established heart disease had blood leptin levels 16% higher than men considered heart healthy. Every 30% increase in leptin increased the risk of a heart attack or a vascular event by 25% (Wallace et al 2001).
With insulin resistance, you no longer have insulin sensitivity. When you are insulin sensitive, you only need to secrete a small amount of insulin to get glucose (glycogen) into the muscles and liver.
Researchers have discovered that a proper diet and regular exercise have the greatest impact on reversing the damage done by leptin resistance. Too little sleep can lower the appetite-control hormone leptin and increase the appetite-stimulating hormone ghrelin. Now research proves that sleep loss may increase dangerous belly fat.
Get a good night’s sleep should be standard doctor’s orders but sleep does not come on command for a large segment of people.
Melatonin, the hormone that regulates your body’s internal clock, is closely linked with leptin production. Your body produces the most leptin overnight while you sleep. Anything that disrupts your sleep can disrupt leptin production.
 Nothing will disturb sleep more than a serious magnesium deficiency, except for pharmaceutical medications for sleep disorders.
Nothing will disturb sleep more than a serious magnesium deficiency, except for pharmaceutical medications for sleep disorders.
It is vitally important to sleep in the dark – any artificial light sources will seriously curtail melatonin production during sleep.
Magnesium
One potential cause for lower serum magnesium in obese youth is low dietary magnesium intake. Studies do show that the calorie-adjusted magnesium intake in obese children was lower compared with lean children. Hypomagnesemia (serum magnesium 0.78 mmol/l) was present in 27% of healthy lean children and 55% of obese children.[8]
One of the causes of magnesium deficiency is over-medicating with synthetic pharmaceutical drugs approved by the FDA and prescribed by doctors. They prevent the body from absorbing magnesium.
It’s a cruel reality that diabetics are prescribed medicines that further reduce their magnesium reserves putting them into a fatal tailspin.
The body requires magnesium to absorb and utilize nutrients. Without magnesium our bodies cannot properly use the fats, proteins and carbohydrates we eat every day.
When we aren’t getting what we need from our diet, we will CRAVE more food in an effort to obtain those vital nutrients.
The body does so by activating hundreds of enzymes in the body. Magnesium helps you get the most from what you eat so you can be satisfied with no more than the amount of food you genuinely need.
Since conditions like insulin resistance and diabetes are strongly associated with obesity, controlling blood sugar levels is a key factor in maintaining a healthy weight. When enough magnesium is present in the body, insulin can function properly and blood glucose is used for energy. A magnesium deficiency causes insulin to function poorly, resulting in high blood sugar and fat storage.
Magnesium is a co-factor of many enzymes involved in glucose metabolism. Magnesium has an important role in insulin action, and insulin stimulates magnesium uptake in insulin-sensitive tissues. Magnesium is required for both proper glucose utilization and insulin signaling. Metabolic alterations in cellular magnesium, which may play the role of a second messenger for insulin action, contribute to insulin resistance.
Magnesium is needed to extract energy from food and for optimal insulin function. The more energy you extract from food the less you have to eat to feel great.
There are co-factors that the body needs in order to utilize vitamin D properly. Magnesium is the most important co-factor for vitamin D. In fact, it is common for rising vitamin D levels to exacerbate an underlying magnesium deficiency.
If one is having difficulty maintaining vitamin D levels, a magnesium deficiency could be the reason.
Magnesium is a mineral that is essential to all cells of all known living organisms. We also see research showing that low serum magnesium levels can be raised by injections of vitamin D. Vitamin D supplementation of 2000 mg/day also reduces the incidence of type-2 diabetes.
The Digestive System and Kidneys
The health status of the digestive system and the kidneys has a significant influence upon the magnesium status. Magnesium is absorbed in the intestines and then transported through the blood to cells and tissues.
Approximately one-third to one-half of dietary magnesium is absorbed into the body. Gastrointestinal disorders that impair absorption such as Crohn’s disease can limit the body’s ability to absorb magnesium. These disorders can deplete the body’s stores of magnesium and in extreme cases may result in magnesium deficiency. Chronic or excessive vomiting and diarrhea may also result in magnesium depletion.
Healthy kidneys are able to limit urinary excretion of magnesium to make up for low dietary intake. However, excessive loss of magnesium in urine can be a side effect of some medications and can also occur in cases of poorly-controlled diabetes and alcohol abuse.
Early signs of magnesium deficiency
include loss of appetite, nausea, vomiting, fatigue, and weakness. As magnesium deficiency worsens, numbness, tingling, muscle contractions and cramps, restless legs, seizures (sudden changes in behaviors caused by excessive electrical activity in the brain), personality changes, abnormal heart rhythms, and coronary spasms can occur.
Severe magnesium deficiency can result in low levels of calcium in the blood (hypocalcemia). Magnesium deficiency is also associated with low levels of potassium in the blood (hypokalemia).  Many of these symptoms are general and can result from a variety of medical conditions other than magnesium deficiency. It is important to have a physician evaluate health complaints and problems so that appropriate care can be given.
Many of these symptoms are general and can result from a variety of medical conditions other than magnesium deficiency. It is important to have a physician evaluate health complaints and problems so that appropriate care can be given.
Stress
Stress management is one of the most important keys in fighting obesity, and magnesium is a vital nutrient for reducing stress. This is because magnesium supports healthy adrenal glands. These are the glands that control the release of adrenaline and cortisol, two hormones related to the stress response. While these hormones are vital to living, too much of them can cause weight gain and other health problems. Magnesium helps regulate these hormones so they are not overproduced.
Magnesium also regulates nervous system response. When we have a magnesium deficiency, our nervous system is over-stimulated, leading to irritation, nervousness and stress. When there is plenty of magnesium, the mind and body are finally able to relax and reverse the effects of stress.
Optimizing hormone levels is critical because hormones influence our moods, thought patterns (negative and positive), behaviors, appearance, and our ability to handle stress.
“Eating throws powerful hormonal switches and WHEN you eat is just as important as WHAT you eat,”
Leptin affects food intake and body weight by actions on the hypothalamus.
Although leptin resistance is common in obesity, mechanisms have not been identified. Speculation holds that the consumption of high amounts of fructose causes leptin resistance and elevated triglycerides in rats. It’s been suggested that the major physiological role of leptin is not as a “satiety signal” to prevent obesity in times of energy excess, but as a “starvation signal” to maintain adequate fat stores for survival during times of energy deficit and that leptin resistance in overweight individuals is the standard feature of mammalian physiology which possibly confers a survival advantage
Magnesium Deficiency Is Associated With Insulin Resistance in Obese Children.
- Magnesium: What is it? Magnesium is the fourth most abundant mineral in the body and is essential to good health. Approximately 50% of total body magnesium is found in bone. The other half is found predominantly inside cells of body tissues and organs. Only 1% of magnesium is found in blood, however, the body works very hard to keep blood levels of magnesium constant.
- Magnesium is needed for more than 300 biochemical reactions in the body. It helps maintain normal muscle and nerve function, keeps heart rhythm steady, supports a healthy immune system, and keeps bones strong. Magnesium also helps regulate blood sugar levels, promotes normal blood pressure, and is known to be involved in energy metabolism and protein synthesis.
- There is an increased interest in the role of magnesium in preventing and managing disorders such as hypertension, cardiovascular disease, and diabetes. Dietary magnesium is absorbed in the small intestines. Magnesium is excreted through the kidneys
What foods provide magnesium?
- Green vegetables such as spinach are good sources of magnesium because the center of the chlorophyll molecule (which gives green vegetables their color) contains magnesium. Some legumes (beans and peas), nuts and seeds, and whole, unrefined grains are also good sources of magnesium. Refined grains are generally low in magnesium. When white flour is refined and processed, the magnesium-rich germ and bran are removed. Bread made from whole grain wheat flour provides more magnesium than bread made from white refined flour. Tap water can be a source of magnesium, but the amount varies according to the water supply. Water that naturally contains more minerals is described as “hard”. “Hard” water contains more magnesium than “soft” water.
Eating a wide variety of legumes, nuts, whole grains, and vegetables will help you meet your daily dietary need for magnesium. Selected food sources of magnesium are listed in Table 1.
Table 1: Selected food sources of magnesiumFOOD Milligrams (mg) %DV* Halibut, cooked, 3 ounces 90 20 Almonds, dry roasted, 1 ounce 80 20 Cashews, dry roasted, 1 ounce 75 20 Soybeans, mature, cooked, ½ cup 75 20 Spinach, frozen, cooked, ½ cup 75 20 Nuts, mixed, dry roasted, 1 ounce 65 15 Cereal, shredded wheat, 2 rectangular biscuits 55 15 Oatmeal, instant, fortified, prepared w/ water, 1 cup 55 15 Potato, baked w/ skin, 1 medium 50 15 Peanuts, dry roasted, 1 ounce 50 15 Peanut butter, smooth, 2 Tablespoons 50 15 Wheat Bran, crude, 2 Tablespoons 45 10 Blackeyed Peas, cooked, ½ cup 45 10 Yogurt, plain, skim milk, 8 fluid ounces 45 10 Bran Flakes, ½ cup 40 10 Vegetarian Baked Beans, ½ cup 40 10 Rice, brown, long-grained, cooked, ½ cup 40 10 Lentils, mature seeds, cooked, ½ cup 35 8 Avocado, California, ½ cup pureed 35 8 Kidney Beans, canned, ½ cup 35 8 Pinto Beans, cooked, ½ cup 35 8 Wheat Germ, crude, 2 Tablespoons 35 8 Chocolate milk, 1 cup 33 8 Banana, raw, 1 medium 30 8 Milk Chocolate candy bar, 1.5 ounce bar 28 8 Milk, reduced fat (2%) or fat free, 1 cup 27 8 Bread, whole wheat, commercially prepared, 1 slice 25 6 Raisins, seedless, ½ cup packed 25 6 Whole Milk, 1 cup 24 6 Chocolate Pudding, 4 ounce ready-to-eat portion 24 6 *DV = Daily Value. DVs are reference numbers developed by the Food and Drug Administration (FDA) to help consumers determine if a food contains a lot or a little of a specific nutrient. The DV for magnesium is 400 milligrams (mg). Most food labels do not list a food’s magnesium content. The percent DV (%DV) listed on the table above indicates the percentage of the DV provided in one serving. A food providing 5% of the DV or less per serving is a low source while a food that provides 10-19% of the DV is a good source. A food that provides 20% or more of the DV is high in that nutrient. It is important to remember that foods that provide lower percentages of the DV also contribute to a healthful diet. For foods not listed in this table, please refer to the U.S. Department of Agriculture’s Nutrient Database Web site: https://www.nal.usda.gov/fnic/cgi-bin/nut_search.pl.
What are the Dietary Reference Intakes for magnesium?
Recommendations for magnesium are provided in the Dietary Reference Intakes (DRIs) developed by the Institute of Medicine of the National Academy of Sciences. Dietary Reference Intakes is the general term for a set of reference values used for planning and assessing nutrient intake for healthy people. Three important types of reference values included in the DRIs are Recommended Dietary Allowances (RDA), Adequate Intakes (AI), and Tolerable Upper Intake Levels (UL). The RDA recommends the average daily intake that is sufficient to meet the nutrient requirements of nearly all (97%-98%) healthy people. An AI is set when there is insufficient scientific data available to establish a RDA for specific age/gender groups. AIs meet or exceed the amount needed to maintain a nutritional state of adequacy in nearly all members of a specific age and gender group. The UL, on the other hand, is the maximum daily intake unlikely to result in adverse health effects. Table 2 lists the RDAs for magnesium, in milligrams, for children and adults .
- Table 2: Recommended Dietary Allowances for magnesium for children and adults
Age
(years)Male
(mg/day)Female
(mg/day)Pregnancy
(mg/day)Lactation
(mg/day)1-3 80 80 N/A N/A 4-8 130 130 N/A N/A 9-13 240 240 N/A N/A 14-18 410 360 400 360 19-30 400 310 350 310 31+ 420 320 360 320 There is insufficient information on magnesium to establish a RDA for infants. For infants 0 to 12 months, the DRI is in the form of an Adequate Intake (AI), which is the mean intake of magnesium in healthy, breastfed infants. Table 3 lists the AIs for infants in milligrams (mg)
Table 3: Recommended Adequate Intake for magnesium for infants
Age
(months)Males and Females
(mg/day)0 to 6 30 7 to 12 75 Data from the 1999-2000 National Health and Nutrition Examination Survey suggest that substantial numbers of adults in the United States (US) fail to get recommended amounts of magnesium in their diets. Among adult men and women, the diets of Caucasians have significantly more magnesium than do those of African-Americans. Magnesium intake is lower among older adults in every racial and ethnic group. Among African-American men and Caucasian men and women who take dietary supplements, the intake of magnesium is significantly higher than in those who do not
When can magnesium deficiency occur?
Even though dietary surveys suggest that many Americans do not get recommended amounts of magnesium. There is concern that many people may not have enough body stores of magnesium because dietary intake may not be high enough. Having enough body stores of magnesium may be protective against disorders such as cardiovascular disease and immune dysfunction .
Who may need extra magnesium?
Magnesium supplementation may be indicated when a specific health problem or condition causes an excessive loss of magnesium or limits magnesium absorption.
- Some medicines may result in magnesium deficiency, including certain diuretics, antibiotics, and medications used to treat cancer (anti-neoplastic medication). Examples of these medications are:
- Diuretics: Lasix, Bumex, Edecrin, and hydrochlorothiazide
- Antibiotics: Gentamicin, and Amphotericin
- Anti-neoplastic medication: Cisplatin
- Individuals with poorly-controlled diabetes may benefit from magnesium supplements because of increased magnesium loss in urine associated with hyperglycemia.
- Magnesium supplementation may be indicated for persons with alcoholism. Low blood levels of magnesium occur in 30% to 60% of alcoholics, and in nearly 90% of patients experiencing alcohol withdrawal. Anyone who substitutes alcohol for food will usually have significantly lower magnesium intakes.
- Individuals with chronic malabsorptive problems such as Crohn’s disease, gluten sensitive enteropathy, regional enteritis, and intestinal surgery may lose magnesium through diarrhea and fat malabsorption. Individuals with these conditions may need supplemental magnesium.
- Individuals with chronically low blood levels of potassium and calcium may have an underlying problem with magnesium deficiency. Magnesium supplements may help correct the potassium and calcium deficiencies.
- Older adults are at increased risk for magnesium deficiency. The 1999-2000 and 1998-94 National Health and Nutrition Examination Surveys suggest that older adults have lower dietary intakes of magnesium than younger adults. In addition, magnesium absorption decreases and renal excretion of magnesium increases in older adults. Seniors are also more likely to be taking drugs that interact with magnesium. This combination of factors places older adults at risk for magnesium deficiency. It is very important for older adults to get recommended amounts of dietary magnesium.
Doctors can evaluate magnesium status when above-mentioned medical problems occur, and determine the need for magnesium supplementation.
Table 4 describes some important interactions between certain drugs and magnesium. These interactions may result in higher or lower levels of magnesium, or may influence absorption of the medication.
Table 4: Common and important magnesium/drug interactions
| Drug | Potential Interaction |
|---|---|
| These drugs may increase the loss of magnesium in urine. Thus, taking these medications for long periods of time may contribute to magnesium depletion |
| Magnesium binds tetracycline in the gut and decreases the absorption of tetracycline. |
| Many antacids and laxatives contain magnesium. When frequently taken in large doses, these drugs can inadvertently lead to excessive magnesium consumption and hypermagnesemia, which refers to elevated levels of magnesium in blood. |
What is the best way to get extra magnesium?
Eating a variety of whole grains, legumes, and vegetables (especially dark-green, leafy vegetables) every day will help provide recommended intakes of magnesium and maintain normal storage levels of this mineral. Increasing dietary intake of magnesium can often restore mildly depleted magnesium levels. However, increasing dietary intake of magnesium may not be enough to restore very low magnesium levels to normal. 
When blood levels of magnesium are very low, intravenous (i.e. by IV) magnesium replacement is usually recommended. Magnesium tablets also may be prescribed, although some forms can cause diarrhea.
It is important to have the cause, severity, and consequences of low blood levels of magnesium evaluated by a physician, who can recommend the best way to restore magnesium levels to normal.
Because people with kidney disease may not be able to excrete excess amounts of magnesium, they should not take magnesium supplements unless prescribed by a physician.
Oral magnesium supplements combine magnesium with another substance such as a salt. Examples of magnesium supplements include magnesium oxide, magnesium sulfate, and magnesium carbonate.
Elemental magnesium refers to the amount of magnesium in each compound. Figure 1 compares the amount of elemental magnesium in different types of magnesium supplements. The amount of elemental magnesium in a compound and its bio-availability influence the effectiveness of the magnesium supplement.
Bio-availability refers to the amount of magnesium in food, medications, and supplements that is absorbed in the intestines and ultimately available for biological activity in your cells and tissues. Enteric coating (the outer layer of a tablet or capsule that allows it to pass through the stomach and be dissolved in the small intestine) of a magnesium compound can decrease bio-availability.
In a study that compared four forms of magnesium preparations, results suggested lower bio-availability of magnesium oxide, with significantly higher and equal absorption and bio-availability of magnesium chloride and magnesium lactate. This supports the belief that both the magnesium content of a dietary supplement and its bioavailability contribute to its ability to restore deficient levels of magnesium.
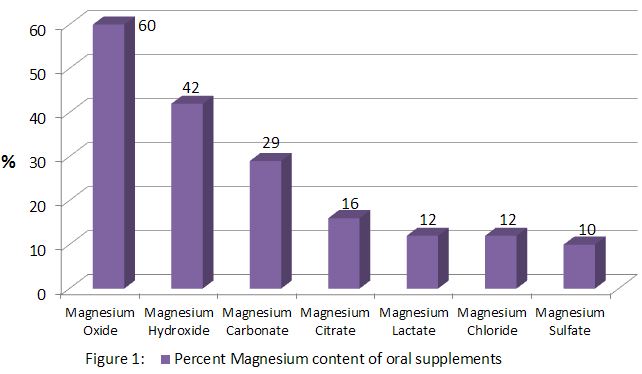
The information in Figure 1 is provided to demonstrate the variable amount of magnesium in magnesium supplements.
What are some current issues and controversies about magnesium?
Magnesium and blood pressure
“Epidemiologic evidence suggests that magnesium may play an important role in regulating blood pressure.” Diets that provide plenty of fruits and vegetables, which are good sources of potassium and magnesium, are consistently associated with lower blood pressure. The DASH study (Dietary Approaches to Stop Hypertension), a human clinical trial, suggested that high blood pressure could be significantly lowered by a diet that emphasizes fruits, vegetables, and low fat dairy foods. Such a diet will be high in magnesium, potassium, and calcium, and low in sodium and fat.
An observational study examined the effect of various nutritional factors on incidence of high blood pressure in over 30,000 US male health professionals. After four years of follow-up, it was found that a lower risk of hypertension was associated with dietary patterns that provided more magnesium, potassium, and dietary fiber.
For 6 years, the Atherosclerosis Risk in Communities (ARIC) Study followed approximately 8,000 men and women who were initially free of hypertension. In this study, the risk of developing hypertension decreased as dietary magnesium intake increased in women, but not in men.
Foods high in magnesium are frequently high in potassium and dietary fiber. This makes it difficult to evaluate the independent effect of magnesium on blood pressure. However, newer scientific evidence from DASH clinical trials is strong enough that the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure states that diets that provide plenty of magnesium are positive lifestyle modifications for individuals with hypertension. This group recommends the DASH diet as a beneficial eating plan for people with hypertension and for those with “prehypertension” who desire to prevent high blood pressure https://www.nhlbi.nih.gov/health/public/heart/hbp/dash/.
Magnesium and diabetes
Diabetes is a disease resulting in insufficient production and/or inefficient use of insulin. Insulin is a hormone made by the pancreas. Insulin helps convert sugar and starches in food into energy to sustain life.
There are two types of diabetes: type 1 and type 2. Type 1 diabetes is most often diagnosed in children and adolescents, and results from the body’s inability to make insulin. Type 2 diabetes, which is sometimes referred  to as adult-onset diabetes, is the most common form of diabetes. It is usually seen in adults and is most often associated with an inability to use the insulin made by the pancreas.
to as adult-onset diabetes, is the most common form of diabetes. It is usually seen in adults and is most often associated with an inability to use the insulin made by the pancreas.
Obesity is a risk factor for developing type 2 diabetes. In recent years, rates of type 2 diabetes have increased along with the rising rates of obesity.
Magnesium plays an important role in carbohydrate metabolism.
It may influence the release and activity of insulin, the hormone that helps control blood glucose (sugar) levels. Low blood levels of magnesium (hypomagnesemia) are frequently seen in individuals with type 2 diabetes.
Hypomagnesemia may worsen insulin resistance, a condition that often precedes diabetes, or may be a consequence of insulin resistance. Individuals with insulin resistance do not use insulin efficiently and require greater amounts of insulin to maintain blood sugar within normal levels.
The kidneys possibly lose their ability to retain magnesium during periods of severe hyperglycemia (significantly elevated blood glucose). The increased loss of magnesium in urine may then result in lower blood levels of magnesium. In older adults, correcting magnesium depletion may improve insulin response and action.
Studies with over 127,000 participants (85,060 women and 42,872 men) with no history of diabetes, cardiovascular disease, or cancer at baseline were followed to examine risk factors for developing type 2 diabetes. Women were followed for 18 years; men were followed for 12 years. Over time, the risk for developing type 2 diabetes was greater in men and women with a lower magnesium intake. This study supports the dietary recommendation to increase consumption of major food sources of magnesium, such as whole grains, nuts, and green leafy vegetables.
Supplemental magnesium on control of type 2 diabetes. In one such study, 63 subjects with below normal serum magnesium levels received either 2.5 grams of oral magnesium chloride daily “in liquid form” (providing 300 mg elemental magnesium per day) or a placebo. At the end of the 16-week study period, those who received the magnesium supplement had higher blood levels of magnesium and improved control of diabetes, as suggested by lower hemoglobin A1C levels, than those who received a placebo. Hemoglobin A1C is a test that measures overall control of blood glucose over the previous 2 to 3 months, and is considered by many doctors to be the single most important blood test for diabetics.
Magnesium and cardiovascular disease
Magnesium metabolism is very important to insulin sensitivity and blood pressure regulation, and magnesium deficiency is common in individuals with diabetes. The observed associations between magnesium metabolism, diabetes, and high blood pressure increase the likelihood that magnesium metabolism may influence cardiovascular disease.
Some observational surveys have associated higher blood levels of magnesium with lower risk of coronary heart disease. In addition, some dietary surveys have suggested that a higher magnesium intake may reduce the risk of having a stroke. There is also evidence that low body stores of magnesium increase the risk of abnormal heart rhythms, which may increase the risk of complications after a heart attack. These studies suggest that consuming recommended amounts of magnesium may be beneficial to the cardiovascular system. They have also prompted interest in clinical trials to determine the effect of magnesium supplements on cardiovascular disease.
Several small studies suggest that magnesium supplementation may improve clinical outcomes in individuals with coronary disease. In one of these studies, the effect of magnesium supplementation on exercise tolerance (the ability to walk on a treadmill or ride a bicycle), chest pain caused by exercise, and quality of life was examined in 187 patients. Patients received either a placebo or a supplement providing 365 milligrams of magnesium citrate twice daily for 6 months. At the end of the study period researchers found that magnesium therapy significantly increased magnesium levels. Patients receiving magnesium had a 14 percent improvement in exercise duration as compared to no change in the placebo group.
Those receiving magnesium were also less likely to experience chest pain caused by exercise.
 In another study, 50 men and women with stable coronary disease were randomized to receive either a placebo or a magnesium supplement that provided 342 mg magnesium oxide twice daily. After 6 months, those who received the oral magnesium supplement were found to have improved exercise tolerance.
In another study, 50 men and women with stable coronary disease were randomized to receive either a placebo or a magnesium supplement that provided 342 mg magnesium oxide twice daily. After 6 months, those who received the oral magnesium supplement were found to have improved exercise tolerance.
In a third study, researchers examined whether magnesium supplementation would add to the anti-thrombotic (anti-clotting) effects of aspirin in 42 coronary patients. For three months, each patient received either a placebo or a supplement with 400 mg of magnesium oxide two to three times daily. After a four-week break without any treatment, treatment groups were reversed so that each person in the study then received the alternate treatment for three months. Researchers found that supplemental magnesium did provide an additional anti-thrombotic effect.
These studies are encouraging, but involved small numbers. Additional studies are needed to better understand the complex relationships between magnesium intake, indicators of magnesium status, and heart disease. Doctors can evaluate magnesium status when above-mentioned medical problems occur, and determine the need for magnesium supplementation.
Magnesium and osteoporosis
Bone health is supported by many factors, most notably calcium and vitamin D. However, some evidence suggests that magnesium deficiency may be an additional risk factor for postmenopausal osteoporosis. 
This may be due to the fact that magnesium deficiency alters calcium metabolism and the hormones that regulate calcium (20). Several human studies have suggested that magnesium supplementation may improve bone mineral density. In a study of older adults, a greater magnesium intake maintained bone mineral density to a greater degree than a lower magnesium intake. Diets that provide recommended levels of magnesium are beneficial for bone health, but further investigation on the role of magnesium in bone metabolism and osteoporosis is needed.
What is the health risk of too much magnesium?
Dietary magnesium does not pose a health risk, however pharmacologic doses of magnesium in supplements can promote adverse effects such as diarrhea and abdominal cramping. Risk of magnesium toxicity increases with kidney failure, when the kidney loses the ability to remove excess magnesium. Very large doses of magnesium-containing laxatives and antacids also have been associated with magnesium toxicity.
For example, a case of hypermagnesemia after unsupervised intake of aluminum magnesia oral suspension occurred after a 16 year old girl decided to take the antacid every two hours rather than four times per day, as prescribed. Three days later, she became unresponsive and demonstrated loss of deep tendon reflex. Doctors were unable to determine her exact magnesium intake, but the young lady presented with blood levels of magnesium five times higher than normal. Therefore, it is important for medical professionals to be aware of the use of any magnesium-containing laxatives or antacids. Signs of excess magnesium can be similar to magnesium deficiency and include changes in mental status, nausea, diarrhea, appetite loss, muscle weakness, difficulty breathing, extremely low blood pressure, and irregular heartbeat.
Table 5 lists the ULs for supplemental magnesium for healthy infants, children, and adults in milligrams (mg). Physicians may prescribe magnesium in higher doses for specific medical problems. There is no UL for dietary intake of magnesium; only for magnesium supplements.
Table 5: Tolerable Upper Intake Levels for supplemental magnesium for children and adults
| Age (years) | Male (mg/day) | Female (mg/day) | Pregnancy (mg/day) | Lactation (mg/day) |
|---|---|---|---|---|
| Infants | Undetermined | Undetermined | N/A | N/A |
| 1-3 | 65 | 65 | N/A | N/A |
| 4 – 8 | 110 | 110 | N/A | N/A |
| 9 – 18 | 350 | 350 | 350 | 350 |
| 19+ | 350 | 350 | 350 | 35 |
Results:
Baseline concentrations of serum Magnesium and 25 hydroxy vitamin D in obese individuals was lower than non obese individuals, the former being significant. Twenty seven percent of obese women versus 15% of non obese women were Magnesium deficient.
Vitamin D injection caused a significant increase in serum Magnesium concentration in obese subjects but not in non obese subjects. There was also a significant increase of serum 25 hydroxy vitamin D in both groups. Mean elevation in serum Magnesium level among women who had Magnesium deficiency was higher than women with Magnesium adequacy.
Conclusion:
Low serum Magnesium concentration in obese individuals can be modified by vitamin D injection
